Introduction:
Most studies on the diagnostic yield of bone marrow biopsy including the one by Hot et al. have focused on the yield of bone marrow biopsies in diagnosing the source of fever of unknown origin. However, there have not been any studies performed to our knowledge looking at overall practice patterns and yield of bone marrow biopsies for diagnoses other than fever of unknown origin. We aim to determine the most common indications for performing bone marrow biopsies in a community-based teaching hospital as well as the yield of the biopsies in patients with specified and unspecified pre-test indications to estimate the rate of uncertain post-test diagnoses.
Methods:
We performed a retrospective data collection study at Rochester General Hospital, NY. A comprehensive search was conducted in our electronic medical data to identify all patients who underwent bone marrow biopsies over a 5 year period from January 2011 - December 2016 for indications other than fever of unknown origin. Patient data including demographics, pre-bone marrow biopsy diagnosis and post-bone marrow diagnosis was obtained. All patients above the age of 18 who underwent bone marrow biopsy for indications other than fever of unknown origin or follow up treatment of a hematological malignancy were included.
Results:
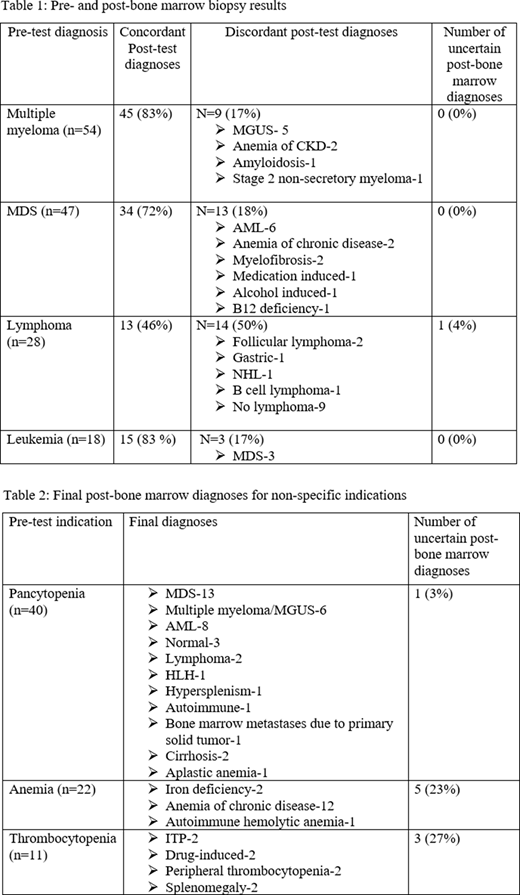
A total of 223 biopsies were performed. The median age was 59 years (age range- 23-95). One hundred and sixteen patients were male and 107 were female. The most common indications for performing bone marrow biopsy were evaluation of the following possible conditions: multiple myeloma (n=54), myelodysplastic syndrome [MDS] (n=47), lymphoma (n=28) and leukemia (n=18) as well as non-specific indications such as pancytopenia (n=40), anemia (n=22) and thrombocytopenia (n=11). The proportion of cases confirmed by bone marrow biopsy was 45/54 (83%) with the pre-marrow diagnosis of multiple myeloma, 34/47 cases (72%) with the pre-marrow diagnosis of MDS, 15/18 (83%) with the pre-marrow diagnosis of leukemia and 13/28 (46%) in those with the pre-marrow diagnosis of rule out lymphoma. Thirteen cases (18%) with possible MDS had post-bone marrow diagnoses of leukemia, anemia of chronic disease, myelofibrosis or medication-related changes. Five out of twenty two cases (23%) for anemia and 3/11 cases (27%) for thrombocytopenia without otherwise specified pre-bone marrow etiology had uncertain diagnosis after bone marrow biopsy.
Conclusion:
In about a fifth of patients necessitating a bone marrow, the diagnosis is discordant and can be surprising. It is also worth reporting that in these discordant results, non-hematological causes such as medications, anemia due to chronic diseases or conditions such as cirrhosis or splenomegaly from other etiologies were among the final diagnoses. Interestingly, 20% of the patients with unspecified pre-bone marrow diagnoses such as anemia or thrombocytopenia in our study had an unclear post-bone marrow diagnosis despite undergoing bone marrow biopsy. Our findings are a reminder that the bone marrow exam does not always lead to a definitive diagnosis and the need by exclusion to include in the differential non-hematological etiologies such as nutritional deficiencies, chronic kidney disease or autoimmune disorders.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal